With 11.4 million prescriptions filled each month, it’s no wonder that the hypertension drug Diovan is one of the most prescribed medications in America. After all, the CDC reports that 1 in 3 adults has high blood pressure.1 In the U.S alone, 67 million people are affected2 —and that’s almost twice the total population of Canada. When you combine all the costs of medications, doctor’s visits, and days missed from work, high blood pressure costs us nearly $50 billion each year.3 It’s a problem.
Most therapies are designed to lower blood pressure by targeting components of the renin-angiotensin system, the signaling cascade that regulates blood pressure and body fluid balance.
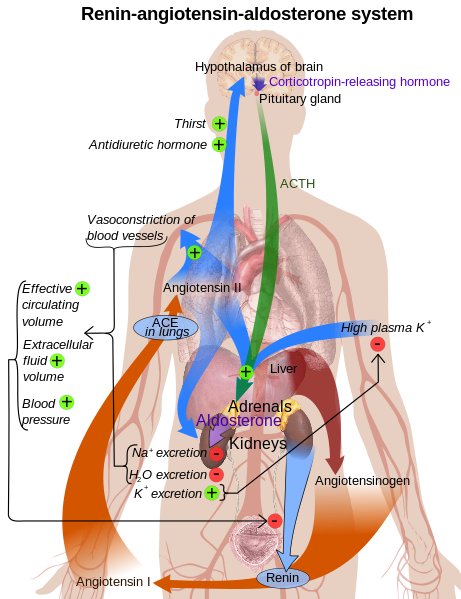
There may be a lot of arrows in this diagram, but it’s actually a simplified version of the renin-angiotensin system. Recent work has exploded, given that these hormones get broken up into smaller peptides (not shown) that all have their own signaling effects!
Normally, this system gets activated when blood pressure is too low, for instance during dehydration or following blood loss. Activation of the renin-angiotensin system increases blood pressure, thus maintaining homeostasis. One of the key steps in this signaling cascade (and thus major target for hypertension drug therapy) is the current gene-of-the-week, ACE (angiotensin converting I enzyme).
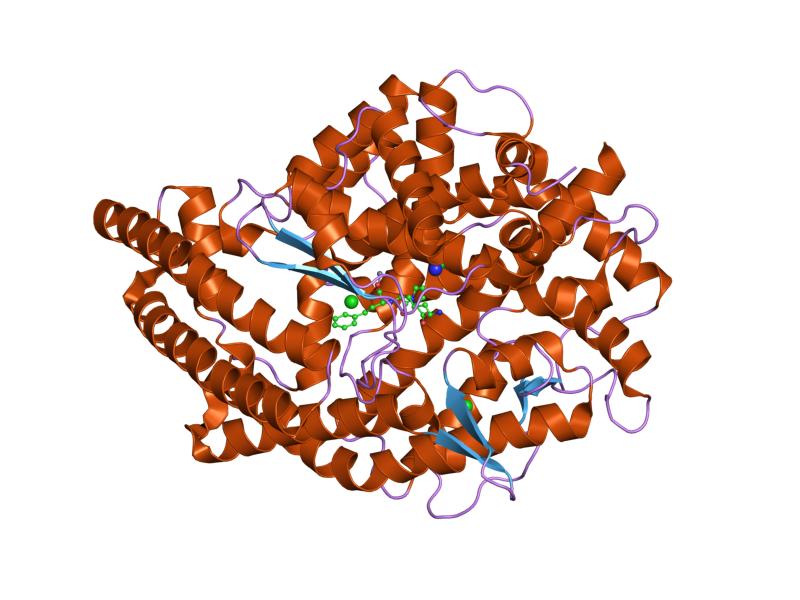
3D structure of ACE.
Activation of ACE eventually increases blood pressure, through its enzymatic role in the conversion of angiotensin I into angiotensin II. Angiotensin II is the main effector of the renin-angiotensin system, signaling through its receptor (AT1) and causing the following downstream effects:4
- Vasoconstriction: blood vessels contract, thus increasing blood pressure.
- Anti-diuresis: urine production is inhibited, thus maintaining body fluid content.
- Anti-natriuresis: excretion of sodium in the urine is inhibited, ultimately preventing further reduction in blood pressure. When sodium concentration is reduced in the blood, osmotic forces subsequently push water out of the blood and into the urine—thus lowering blood volume and pressure.
- Aldosterone release: aldosterone is another hormone that further increases blood pressure and volume.
Therefore, ACE inhibitor drugs become attractive (and effective) options for treating hypertension.
Given that healthy cardiovascular function affects the entire body, ACE inhibitor drugs have also been investigated for treatment of other maladies. Indeed, one randomized controlled trial demonstrated that an ACE inhibitor improved exercise capability and mobility in elderly subjects.5 What’s the motivation for this seemingly random (and mechanistically unclear) effect? ACE has further entered into the public spotlight via its potential influence on athletic performance!
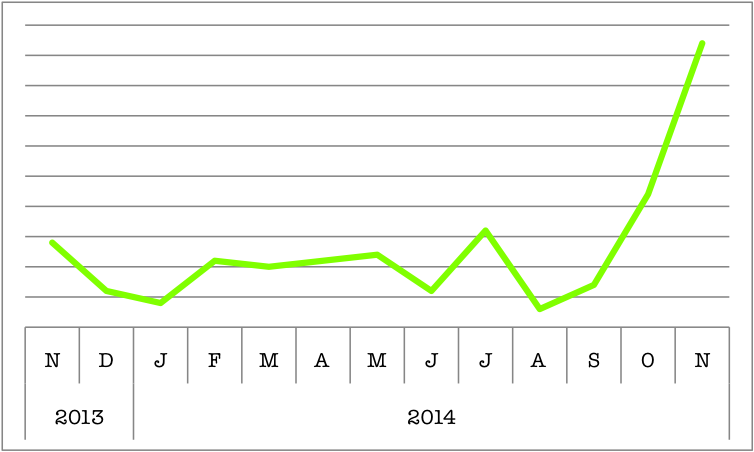
ACE has increased in popularity on BioGPS. The renin-angiotensin system may have been discovered over a century ago, but high blood pressure hasn’t been solved yet—and until then, this gene will remain inherently interesting. More recently though, it’s been implicated in another trendy topic: sport performance.
No one argues that genetics influences your athleticism. (Just look at the Matthews’ family; their football dynasty spans three generations, with a grand total of seven NFL players!) In fact, it’s generally agreed that heritability of “athlete status” is at 66%.6 What remains contentious is the particular genetic polymorphisms that confer this athletic ability. Of the many “sport genes” that have been proposed, ACE is still a popular contender. Just in the past year, there have been eight publications looking at the connection between ACE genetic variants and sport performance! Results haven’t been completely consistent (perhaps owing to inexact comparisons between different sports); still, there’s sufficient evidence to suggest a connection. One gene variant contains a 287bp insertion that lowers ACE activity. This particular polymorphism is more common to Olympic-caliber athletes (like runners and rowers), and is associated with improved performance in endurance sports.7 With just a perfunctory explanation of “increased cardiorespiratory efficiency”, the mechanisms underlying superior athleticism are still undefined. What is obvious though, is that with its connections to hypertension treatment and the elusive “sport gene”, ACE is sure to remain a hot topic for years to come.
REFERENCES:
- “High Blood Pressure Facts.” CDC. Retrieved 12 December 2014 from http://www.cdc.gov/bloodpressure/facts.htm [↩]
- “High Blood Pressure Facts.” CDC. Retrieved 12 December 2014 from http://www.cdc.gov/bloodpressure/facts.htm [↩]
- “High Blood Pressure Facts.” CDC. Retrieved 12 December 2014 from http://www.cdc.gov/bloodpressure/facts.htm [↩]
- Ferrao et al. (2014) Renin-angiotensin system in the kidney: What is new? World J Nephrol 3(3):64-76. [↩]
- Sumukadas et al. (2007) Effect of perindopril on physical function in elderly people with functional impairment: A randomized controlled trial. CMAJ 177(8):867-874. [↩]
- Ma et al. (2013) The association of sport performance with ACE and ACTN3 genetic polymorphisms: A systematic review and meta-analysis. PLoS ONE 8(1): e54685. [↩]
- Ma et al. (2013) The association of sport performance with ACE and ACTN3 genetic polymorphisms: A systematic review and meta-analysis. PLoS ONE 8(1): e54685. [↩]
