Today’s funerary practices might include trends like eco-friendly burial shrouds and artificial reefs made from cremated remains, but for the Fore tribespeople in Papua New Guinea, their traditional mortuary ritual involved a different custom… cannibalism. Although discontinued since the 1960s, the Fore believed that consumption of one’s deceased relatives allowed the departed souls to reach the land of the dead, and be reborn.1 However, this practice unknowingly created the perfect conditions for a severe epidemic of an incurable, debilitating—and fatal—neurological disorder known as kuru.

On the island of New Guinea, circa 1912. (Source: Wikimedia Commons)
Symptoms of kuru (also called the “laughing death”) included not only behavioral changes like inappropriate euphoria and compulsive laughter, but also progressive neurodegeneration that resulted in loss of muscle control, and inevitably (within a year of initial symptoms) death.2 Since kuru victims were nearly all women and children, scientists assumed that the disease carried a genetic or hormonal component.3 In fact, researchers determined that the disease is actually caused by an infectious agent found in the brains of kuru patients—the organs typically eaten by women and children during mortuary rites.4 Decades of research (and two Nobel Prizes) later, these pathogens have been identified as “proteinaceous infectious particles” named prions.
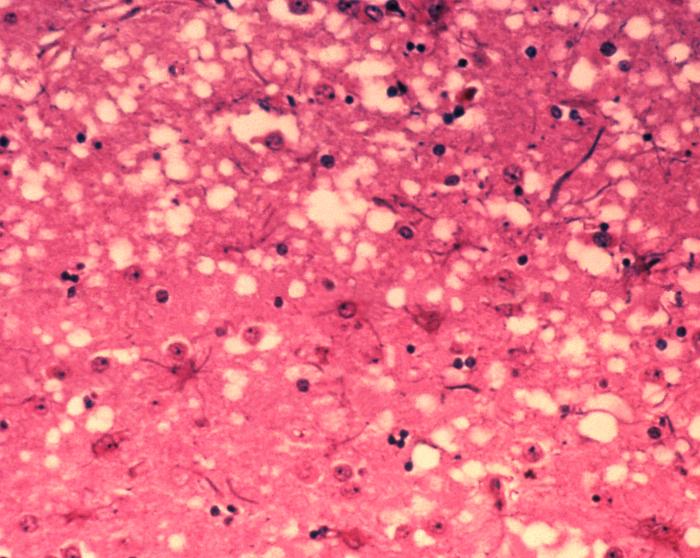
Characteristic pathology of prion diseases includes “holes” in the brain tissue. (Source: Wikimedia Commons)
Encoded by the gene PRNP, normal prion proteins (denoted PrPc, for “common” form) exist naturally in the brain. While the function of normal PrPc protein is still unclear, the misfolded form (PrPsc) is contagious and highly resistant to most sterilization techniques. Unlike most pathogens, misfolded prions propagate by interacting with normal PrPc and causing it to change shape—becoming the PrPsc form. As PrPsc aggregate in the brain, they form stable plaques that disrupt normal tissue structure and eventually lead to neurodegeneration. And while kuru is likely eradicated, prions remain a critical health concern, responsible for an entire class of infectious, fatal neurodegenerative diseases:5
- Creutzfeld-Jakob Disease (CJD): can be caused by an inherited mutation in PRNP gene or, in Variant CJD (vCJD) can be caused by exposure to misfolded PrPsc (e.g. through ingestion or via contaminated surgical tools).
- Gerstmann-Straussler-Scheinker Disease: caused by inherited PRNP gene mutation
- Fatal Familial Insomnia: caused by inherited PRNP gene mutation
- Bovine Spongiform Encephalopathy: the so-called “Mad Cow Disease,” affecting cattle. Misfolded PrPSc is transmittable to humans (thus causing vCJD) via ingestion of contaminated beef. Responsible for inciting a worldwide health scare in the 1990s.
- Scrapie: occurring in sheep. Behavioral symptoms also include itchiness, such that infected sheep will compulsively rub against trees, scraping off their fleece. PrPsc is actually named for its misfolded “Scrapie” form.
- Chronic Wasting Disease (CWD): occurring in deer, elk, and moose. PrPsc is shed in feces, remains in the soil, and can infect other deer that re-ingest that grass.6 It’s uncertain whether prions from CWD can infect humans.
Caused by consumption of PrPsc-contaminated beef, vCJD was first reported in 1996; in response, millions of (potentially-infected) cattle were slaughtered in the UK, and pulled from the food supply.7 Since then, there have been more than 220 documented cases of vCJD, primarily in the UK and France.8 The initial prion (PrPsc) infection was probably transmitted and amplified by feeding cattle a “meat-and-bone meal” comprised of either BSE-infected beef or scrapie-infected sheep meat.9 Now, there are strict bans on using “mammalian-derived proteins” in livestock feed, though many criticize the loophole that still allows use of blood.10
An artistamp commemorating the “Mad Cow Disease” (BSE) epidemic in the UK. (Source: Wikimedia Commons)
Still, with the current government regulations that include routine cattle testing, fear of “Mad Cow disease” has mostly subsided in the general public. In contrast, public health authorities remain concerned by the possibility of another vCJD epidemic; recently, cases of vCJD have been caused by transfusion of contaminated blood!11 Because symptoms of prion disease take so long to manifest (occasionally years) in vCJD patients, their contaminated blood donations can be overlooked. In fact, current estimates indicate that 1:2000 people in the UK may have abnormal prion accumulation.12 Given the difficulty in screening blood donations for PrPsc-contamination, many countries have placed outright restrictions on blood donations from people that have spent significant time in the UK. Development of such a preclinical detection test has been ongoing for nearly a decade, and a new blood-based screening assay shows promise in identifying infected individuals!13

Another public health concern involves proper sterilization of neurosurgery tools, so as not to transmit abnormal prions (PrPSc) between patients! Prions are notoriously difficult to inactivate, and must undergo extra steps beyond normal sterilization procedures. Of course, prions in meat persist throughout the cooking process… (Source: Wikimedia Commons)
Today, decades after their first discovery, prions (PrPsc) are still largely undetectable, nearly indestructible, and thus… utterly terrifying.
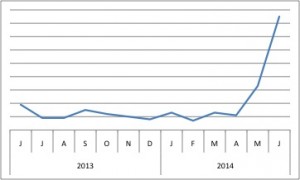
Popularity of PRNP (via BioGPS) increased this past month, coinciding not only with several new publications, but also with the CDC’s announcement of a 4th confirmed vCJD case in the US. The patient was from Texas, but was presumably infected via contaminated meat eaten while traveling overseas. (US status for BSE remains “negligble”.)
However, before you forgo meat and/or all medical procedures, take comfort in the fact that incidence of vCJD is quite low, and that the scientific community is aware of (and actively trying to address) this urgent public health concern. Indeed, in the last month alone, research publications have
- Developed a blood-based test for preclinical detection of PrPsc-infection14
- Proposed an antibody-based treatment that may impair PrPsc propagation15
- And even suggested that caffeine may protect against prion-mediated neurotoxicity!16
So, to all my conflicted meat-lovers and fellow hypochondriacs, try not to let this #GeneOTW ruin your remaining summer BBQs, and instead remember… science is working on a solution!
References:
- Liberski PP, Sikorska B, Lindenbaum S, Goldfarb LG, McLean C, Hainfellner JA, Brown P. (2012) Kuru: genes, cannibals and neuropathology. J Neuropathol Exp Neurol 71(2):92-103. [↩]
- Liberski PP, Sikorska B, Lindenbaum S, Goldfarb LG, McLean C, Hainfellner JA, Brown P. (2012) Kuru: genes, cannibals and neuropathology. J Neuropathol Exp Neurol 71(2):92-103. [↩]
- Liberski PP, Sikorska B, Lindenbaum S, Goldfarb LG, McLean C, Hainfellner JA, Brown P. (2012) Kuru: genes, cannibals and neuropathology. J Neuropathol Exp Neurol 71(2):92-103. [↩]
- Liberski PP, Sikorska B, Lindenbaum S, Goldfarb LG, McLean C, Hainfellner JA, Brown P. (2012) Kuru: genes, cannibals and neuropathology. J Neuropathol Exp Neurol 71(2):92-103. [↩]
- Liberski PP, Sikorska B, Lindenbaum S, Goldfarb LG, McLean C, Hainfellner JA, Brown P. (2012) Kuru: genes, cannibals and neuropathology. J Neuropathol Exp Neurol 71(2):92-103. [↩]
- Giachin G, Narkiewicz J, Scaini D, Ngoc AT, Margon A, Sequi P, Leita L, Legname G. (2014) Prion protein interaction with soil humic substances: environmental implications. PLoS One 9(6):e100016. [↩]
- Confirmed Variant Creutzfeldt-Jakob Disease (variant CJD) Case in Texas. CDC. Retrieved June 6, 2014, from http://www.cdc.gov/ncidod/dvrd/vcjd/other/confirmed-case-in-texas.htm [↩]
- Confirmed Variant Creutzfeldt-Jakob Disease (variant CJD) Case in Texas. CDC. Retrieved June 6, 2014, from http://www.cdc.gov/ncidod/dvrd/vcjd/other/confirmed-case-in-texas.htm [↩]
- BSE (Bovine Spongiform Encephalopathy, or Mad Cow Disease. CDC. Retrieved June 6, 2014, from http://www.cdc.gov/ncidod/dvrd/bse/index.htm [↩]
- Stone, Andrea. 4th Death From Mad Cow Disease Confirmed in U.S. National Geographic. Retrieved June 6, 2014, from http://news.nationalgeographic.com/news/2014/06/140604-world-mad-cow-disease-health-death/ [↩]
- Lacroux C, Comoy E, Moudjou M, Perret-Liaudet A, Lugan S, Litaise C, Simmons H, Jas-Duval C, Lantier I, Béringue V, Groschup M, Fichet G,Costes P, Streichenberger N, Lantier F, Deslys JP, Vilette D, Andréoletti O. (2014) Preclinical Detection of Variant CJD and BSE Prions in Blood. PLoS Pathog10(6):e1004202. [↩]
- Lacroux C, Comoy E, Moudjou M, Perret-Liaudet A, Lugan S, Litaise C, Simmons H, Jas-Duval C, Lantier I, Béringue V, Groschup M, Fichet G,Costes P, Streichenberger N, Lantier F, Deslys JP, Vilette D, Andréoletti O. (2014) Preclinical Detection of Variant CJD and BSE Prions in Blood. PLoS Pathog10(6):e1004202. [↩]
- Lacroux C, Comoy E, Moudjou M, Perret-Liaudet A, Lugan S, Litaise C, Simmons H, Jas-Duval C, Lantier I, Béringue V, Groschup M, Fichet G,Costes P, Streichenberger N, Lantier F, Deslys JP, Vilette D, Andréoletti O. (2014) Preclinical Detection of Variant CJD and BSE Prions in Blood. PLoS Pathog10(6):e1004202. [↩]
- Lacroux C, Comoy E, Moudjou M, Perret-Liaudet A, Lugan S, Litaise C, Simmons H, Jas-Duval C, Lantier I, Béringue V, Groschup M, Fichet G,Costes P, Streichenberger N, Lantier F, Deslys JP, Vilette D, Andréoletti O. (2014) Preclinical Detection of Variant CJD and BSE Prions in Blood. PLoS Pathog10(6):e1004202. [↩]
- David MA, Jones DR, Tayebi M. (2014) Potential candidate camelid antibodies for the treatment of protein-misfolding diseases. J Neuroimmunol272(1-2):76-85. [↩]
- Moon JH, Lee JH, Park JY, Kim SW, Lee YJ, Kang SJ, Seol JW, Ahn DC, Park SY. (2014) Caffeine prevents human prion protein-mediated neurotoxicity through the induction of autophagy. Int J Mol Med34(2):553-8. [↩]

Trackbacks/Pingbacks